At the meeting of the sub-committee in charge of drafting documents for the 14th National Party Congress on March 15, Party General Secretary To Lam raised a pivotal question: “Can we strive to provide free hospital care for the people by 2030?” He then proposed that if feasible, this goal should be added directly to the draft political report for the Congress. This strategic vision has since been reaffirmed by the General Secretary in other working sessions.
The two directions proposed by the General Secretary, including annual health check-ups for all citizens and universal free hospital care, go beyond medical targets. They carry a profound message: “Policy must originate from the people, for the people, and for sustainably developed Viet Nam”. Annual health check-ups for the people are not an unrealistic goal if we have strong political will, broad societal consensus, and a clear and methodical roadmap for implementation.
Deputy Minister of Health Tran Van Thuan
The path to healthcare equity
According to leaders at the Ministry of Health, implementing the policy of universal free hospital care will bring numerous positive impacts, such as expanding access to medical services, proactive prevention, early diagnosis and treatment, improving treatment outcomes, optimising healthcare resources, reducing the financial burden on citizens. This, in turn, increases opportunities for poverty alleviation, improves the quality of human resources, boosts labour productivity, contributes to national GDP growth, minimises the risk of economic lag, and ultimately promotes greater social equity.
From the perspective of a frontline medical institution, Associate Professor Dr Dao Xuan Co, Director of Bach Mai Hospital in Ha Noi, emotionally recalled the sight of impoverished patients in critical condition who were forced to go to higher-level hospitals for treatment, leaving their families financially devastated. Many families, he noted, fell back into poverty after just one hospitalisation, even after having recently escaped it. Therefore, upon hearing General Secretary To Lam’s resolute commitment to nationwide free hospital care, he viewed it as a revolutionary step for Viet Nam's healthcare system. With efficient resource coordination and consistent political will, he believes this goal is entirely achievable.
“Three pillars for successful realisation of this ambitious policy are comprehensive and diversified universal health insurance coverage; robust public investment in healthcare, especially in disadvantaged regions; and mobilised support from businesses and charitable organisations,” emphasised Dr Co. “We should also learn from the non-profit hospital models in many developed countries.”
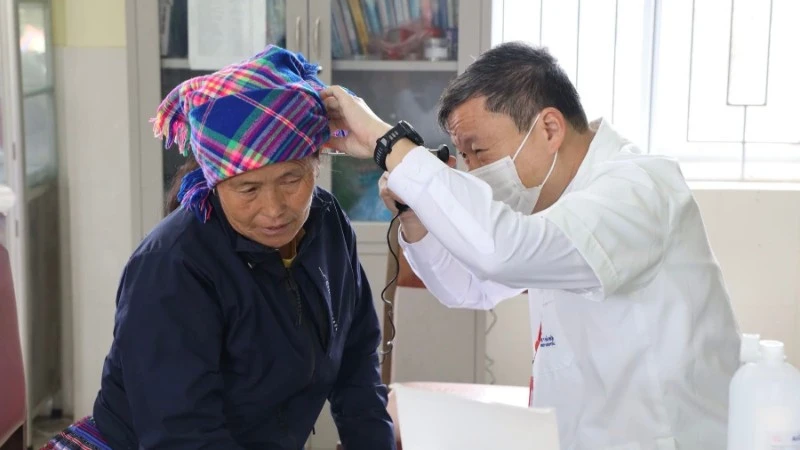
To ensure no one is left behind, grassroots healthcare systems need the strongest support. Local healthcare workers must be multi-skilled, responsive to real needs, and preferably recruited from their communities to ensure long-term commitment. Compensation policies and working conditions must be fundamentally improved. These frontline workers need proper medical supplies, equipment for effective diagnosis and treatment, and a living wage to sustain their dedication. Digital technologies, such as electronic health records, can provide critical support to grassroots healthcare facilities, helping to reduce the burden on central hospitals. Dr Co said: “Free hospital fees not only reduces patient expenses but also changes the mindset of comprehensive healthcare, placing humans at the centre of development. With regular check-ups, early detection, and timely treatment, we shift from treatment to prevention, from being reactive to being proactive”.
Sharing this view, Tran Thanh Tung from Ha Noi Medical University emphasised that health insurance plays a vital role in reducing financial strain for patients, especially those from disadvantaged backgrounds. “We must aim for universal health insurance coverage to ensure everyone receives equal support. The state budget can fully subsidise health insurance costs for the poor, which is a practical solution to improving public healthcare,” Tung affirmed.
A comprehensive strategy to expand coverage
To translate the universal free hospital care policy into reality, Professor Dr Nguyen Anh Tri, a National Assembly deputy, stressed the need for coordinated and integrated funding mechanisms, closely linked to the national health insurance system. In other words, the goal of free hospital care can be achieved through comprehensive health insurance coverage. He emphasised that if every citizen holds a health insurance card, they can access medical services without worrying about the cost. Therefore, it is essential to consider increasing subsidies for health insurance premiums, especially for vulnerable groups.
The Professor also proposed a detailed roadmap, with phased implementation based on priority groups, to realise universal free hospital care by 2030. The initial priority should be given to people with meritorious service, war invalids, families of martyrs, children under six, patients with chronic or life-threatening conditions, and the elderly. These groups could begin receiving free hospital care starting in 2026, with gradual expansion to other groups, aiming to achieve nationwide coverage by 2030.
Many experts also agreed on the necessity of a clear roadmap, inter-agency consensus, and thorough preparation in terms of infrastructure, human resources, and funding. Particularly, integration with the health insurance system would help gradually expand both benefit levels and the range of services covered, while supporting the cost of premiums for low-income, elderly, or disadvantaged groups to reduce out-of-pocket expenses. It is also vital to clearly define the maximum level of support, the list of free medicines and services, and the oversight mechanisms to prevent corruption, abuse, or profiteering. In parallel, a voluntary care system should be maintained, allowing citizens to pay for enhanced services alongside the free basic package.
Sharing international perspectives, Dr Angela Pratt, WHO Representative in Viet Nam, stressed the urgency of a comprehensive, coordinated, and sustainable national strategy. She also expressed her support for the Vietnamese Government’s policy. It reflects a long-term healthcare vision and the State’s strong commitment to building a healthier and happier Viet Nam.
However, Dr Pratt also cautioned that as public healthcare funding increases, out-of-pocket payments by individuals should be limited to a reasonable co-payment level. She added that there should be clear regulations for non-medical expenses such as optional services, meals, and personal amenities. Another strategic element is how the healthcare system is structured. WHO recommends putting primary healthcare at the centre.
According to estimates from the Ministry of Finance and WHO, Viet Nam’s public health expenditure currently accounts for around 2.9% of GDP. If this rises to 4% within five years and 5% within ten years, the country could reduce out-of-pocket health expenses to below 20%, moving closer to the goal of free basic healthcare. However, Dr Pratt warned that merely increasing the health budget is not enough without accompanying systemic reforms. These should include regulating service prices, avoiding overuse of expensive technologies, enhancing oversight, and improving the quality of care at grassroots levels.
In terms of human resources, as of 2023, Viet Nam had approximately 514,000 healthcare workers, including nearly 100,000 doctors, about 11 doctors per 10,000 people, comparable to many similarly developed countries. However, workforce distribution remains uneven, with high workloads and low pay prompting many doctors to leave the public sector or seek opportunities abroad. While Viet Nam’s healthcare workforce is something to be proud of, retaining them in the public system requires a transparent, performance-based compensation mechanism. A fair pay structure will not only encourage professional integrity but also improve service quality.
Universal free hospital care is a humanitarian turning point that reflects a strong commitment to building a healthy and equitable Viet Nam. If implemented effectively, it will be a historic breakthrough, ensuring that every citizen receives medical care without the burden of financial hardship.
- During the 2026–2030 period, the Ministry of Health will pilot expanded health insurance benefits, increase reimbursement rates, offer annual health check-ups, and establish specialised funds within the national insurance system.
- During the 2030–2035 period, the Law on Health Insurance will be comprehensively revised, aiming to eliminate patient co-payments at primary healthcare facilities.
- By 2045, a modern and equitable healthcare system will be developed so that every citizen receives free medical care without any co-payment.
In the world, about 72 countries have implemented universal healthcare systems, covering at least 90% of their populations. Cuba’s public health system, established after the 1959 Revolution, is entirely free. The state owns all healthcare facilities, with no private hospitals, guaranteeing citizens access to medical consultations, pharmaceuticals, dental and ophthalmological treatments at no cost. Cuba places strong emphasis on preventive care, with a nationwide network of community doctors. As a result, despite being a low-income nation, Cuba has achieved health indicators on par with developed countries.